Breast Reduction Surgery and Breastfeeding: What You Need to Know
Breast reduction surgery, or reduction mammaplasty, is a widely performed procedure aimed at alleviating physical discomfort caused by overly large breasts. Women with macromastia often experience back, neck, and shoulder pain, skin irritation beneath the breast fold, posture problems, and limitations in physical activity. Beyond these physical concerns, many patients also seek breast reduction for aesthetic reasons, desiring a breast size that is proportional to their body. However, a common question that arises before undergoing this surgery is whether breastfeeding will still be possible afterward.
How Breast Reduction Surgery Affects Lactation
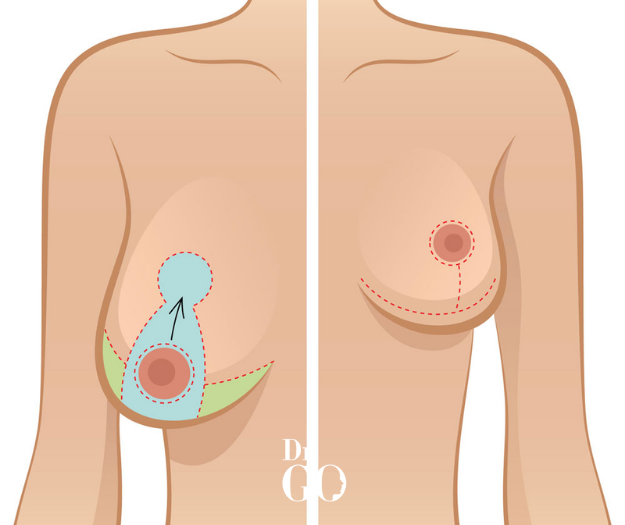
The impact of breast reduction on breastfeeding largely depends on the surgical technique used and the amount of tissue removed. Modern reduction procedures prioritize preservation of the nipple-areola complex along with its nerve and blood supply, which is critical for successful lactation. Techniques such as the superior pedicle, inferior pedicle, or medial pedicle methods are commonly employed to maximize the likelihood of breastfeeding after surgery.
Despite these precautions, it is important to recognize that some reduction methods involve more extensive tissue removal or may disrupt milk ducts. In such cases, milk production may be reduced, and, rarely, breastfeeding may become impossible. The degree of effect varies among patients depending on factors such as the original breast size, the chosen surgical approach, and individual anatomical differences.
Timing Surgery and Pregnancy
For women planning future pregnancies, it is advisable to consider the timing of breast reduction carefully. Ideally, surgery should be performed before pregnancy to relieve pre-existing discomfort and improve quality of life. However, women who have had children and plan to breastfeed in the future can still undergo reduction mammaplasty, provided the surgical approach is tailored to preserve the nipple-areola complex and milk ducts. Discussing reproductive plans with a qualified plastic surgeon ensures that the selected technique balances both aesthetic goals and potential lactation outcomes.
Postoperative Recovery and Breastfeeding
Recovery after breast reduction typically involves some swelling, bruising, and temporary numbness, which gradually resolve over several weeks. Patients are advised to follow postoperative care instructions carefully to promote healing and minimize complications. Once breastfeeding, it is common to encounter challenges such as nipple tenderness, engorgement, or difficulty with the baby latching. These issues are often manageable with guidance from a lactation consultant, who can provide techniques and strategies to maximize milk supply and ensure effective feeding.
Considerations for Long-Term Lactation
While many women successfully breastfeed after reduction surgery, it is important to maintain realistic expectations. Minor reductions in milk production are possible, particularly in cases of extensive tissue removal. Regular monitoring of infant growth and feeding patterns is essential to ensure that the baby is receiving adequate nutrition. In some instances, partial supplementation may be necessary, but this does not diminish the significant physical and psychological benefits of breast reduction surgery.
Conclusion
Breast reduction surgery offers substantial relief from physical discomfort while enhancing aesthetic proportions. With modern surgical techniques that carefully preserve the nipple-areola complex and key milk ducts, many patients retain the ability to breastfeed successfully. Open communication with a board-certified plastic surgeon is essential to select the most appropriate surgical approach, set realistic expectations, and achieve both optimal breast appearance and functional lactation outcomes. By understanding the relationship between reduction surgery and breastfeeding, women can make informed decisions that improve quality of life while maintaining the possibility of nurturing their children in the future.